Beginning in 2010, USAID’s Bureau for Africa has reviewed the progress of family planning programs in USAID priority countries in SSA at regular five-year intervals. Section 2 of our report updates the 2016 analysis Fostering Economic Growth, Equity, and Resilience in Sub-Saharan Africa: The Role of Family Planning, with a continued focus on the 22 USAID priority countries in the region, which represent about three-quarters of SSA’s population.
Since the Bureau of Africa first undertook regular program reviews beginning in 2010, the global measurement landscape has changed significantly. Measurement approaches that historically focused exclusively on population-level indicators of progress―such as “new family planning users” or the modern contraceptive prevalence rate (mCPR)―are being reimagined, with greater attention to more person-centered metrics of program progress that prioritize client satisfaction, choice, and autonomy. Until such metrics are systematically integrated into nationally representative data collection efforts, mCPR remains the primary benchmark of program progress in many countries.
Section 2’s analysis retains the metric annual average percentage-point increase in mCPR between the last two surveys, used in the 2010 and 2016 reports. To reflect drastic changes in the family planning landscape in SSA over the last decade, we examine program progress in the context of countries’ positions along the S-curve from low to high mCPR. This section also supports family planning leaders and stakeholders in their efforts to improve national family planning programs by analyzing results from the National Composite Index for Family Planning (NCIFP) in the context of national commitments made through the FP2020 partnership. Finally, we consider the COVID-19 pandemic as a potential disruptor of family planning program progress.
Modern contraceptive use continues to increase significantly across sub-Saharan Africa.
Countries are organized into four progress categories based on average annual percentage-point increases in mCPR between the two most recent Demographic and Health Surveys (DHS), as shown in Table 1:
-
Rapid Progress (annual mCPR increase of more than 2 percentage points and/or mCPR of ≥ 40%):
Mozambique, Malawi, Kenya, Rwanda, Madagascar, Ethiopia, Zambia.
-
Encouraging Progress (annual mCPR increase of more than 1 and ≤ 2 percentage points):
Uganda, Mali, Niger, Senegala, Guinea.
-
Slow Progress (annual mCPR increase of ≥ 0.5 and ≤ 1.0 percentage point):
Ghana, Burkina Faso, Tanzania, Benin, Liberia, Togo.
-
Little or No Progress (annual mCPR increase of < 0.5 percentage points):
Nigeria, Côte d'Ivoire, Democratic Republic of Congo (DRC).
- No data: South Sudan.
Table 1. Average Annual Percentage-Point Increase in mCPR in Selected Countries in Sub-Saharan Africa
| Rapid Progress (annual increase >2 percentage points and/or mCPR ≥ 40 percent) | ||
|---|---|---|
| Mozambique | 2011-2015 | 3.5 |
| Malawi | 2010-2015/16 | 2.9 |
| Kenya | 2008/09-2014 | 2.5 |
| Rwanda | 2015-2019/20 | 2.4 |
| Madagascar | 2004-2008/09 | 2.2 |
| Ethiopia | 2016-2019 | 1.7 |
| Zambia | 2013/14-2018 | 0.7 |
| Encouraging Progress (annual increase of 1-2 percentage points) | ||
| Uganda | 2011-2016 | 1.8 |
| Mali | 2012/13-2018 | 1.3 |
| Niger | 2006-2012 | 1.2 |
| Senegal | 2014-2019 | 1.0 |
| Guinea | 2012-2018 | 1.0 |
| Slow Progress (annual increase of 0.5-1 percentage points) | ||
| Ghana | 2008-2014 | 0.9 |
| Burkina Faso | 2003-2010 | 0.9 |
| Tanzania | 2010-2015/16 | 0.8 |
| Benin | 2012-2017/18 | 0.8 |
| Liberia | 2013-2019/20 | 0.7 |
| Togo | 1998-2013 | 0.6 |
| No Progress (annual increase of 0-0.4 percentage points) | ||
| Nigeria | 2013-2018 | 0.4 |
| Côte d'Ivoire | 1999-2011/12 | 0.4 |
| DRC | 2007-2013/14 | 0.3 |
Notes: Countries with an mCPR greater than or equal to 40% include Ethiopia, Kenya, Malawi, Rwanda, and Zambia. Senegal is the only country that implements a Continuous DHS. For consistent comparison, we assess the five-year period from the 2014 DHS to the most recent 2019 Continuous DHS. Countries in italics have had no new survey since the 2016 report.
Source: Demographic and Health Surveys; data for Mozambique are from the 2015 AIDS Indicator Survey (AIS).
More than half of USAID priority countries in Sub-Saharan Africa are achieving annual increases in mCPR of at least one percentage point per year or are sustaining a total mCPR over 40%.
Since the 2016 report, Mozambique has entered the Rapid Progress category and Ethiopia has reached an mCPR of more than 40% (40.5%). Mali and Guinea have accelerated increases in mCPR, moving from the Slow and No Progress categories, respectively, into the Encouraging Progress category. Benin has moved from the No Progress category to the Slow Progress category.
In contrast, the pace of mCPR growth has slowed in Senegal and Liberia. Nigeria remains in the No Progress category.
Notably, 10 countries have not conducted or released a new DHS since the 2016 report. The lack of new surveys is partially due to the COVID-19 pandemic, which stalled data collection across the region as countries grappled with mitigating the health and safety risks associated with sending enumerators into local communities. For some countries―including Burkina Faso, Côte d'Ivoire, Madagascar, and Niger―their data are now more than a decade old.
Trends in contraceptive prevalence, both among married women and all women samples, are shown in Figure 1. Overall, mCPR continues to rise across SSA:
- Only one country (DRC) has an mCPR under 10% (DRC has not released a new DHS since 2013/14).
- Twelve countries have mCPRs of more than 20%, compared with eight countries in the last review.
- Seven countries have mCPRs of more than 30%, compared with five countries in the last review.
- Five countries have mCPRs of more than 40%, compared with four countries in the last review.
- Three countries have mCPRs of more than 50%.
Figure 1. mCPR for Married Women and All Women Based on Most Recent Survey, by Overall mCPR
Source: Demographic and Health Surveys.
Most USAID priority countries in SSA have reached a stage where rapid increases in mCPR are possible with the right investments.
Since 2010, the family planning program landscape in SSA has changed drastically. In the context of this change, the indicator of average annual percentage-point increase in mCPR can mask important variations in growth across different programmatic environments.
Historical data based on analyses of family planning trends among married women reveal that mCPR generally grows in an S-shaped pattern, known as the family planning S-curve. The S-curve is characterized by slow growth and little annual change when the mCPR is low (Stage 1); an opportunity for rapid growth during the transition from low to high mCPR (Stage 2); and slow growth as mCPR reaches high levels in a population (Stage 3). While all countries go through this general pattern, the duration and speed of mCPR growth seen in each stage (and, therefore, the specific shape of a country’s curve) varies.4 Understanding the position of countries along the S-curve can inform program priorities and help decisionmakers set ambitious but achievable goals. In this report, we use the S-curve categorization to examine other aspects of program performance in addition to family planning uptake.
When USAID initiated the first Family Planning Program Review in 2010, only 10 priority countries were in Stage 2.b At the time of this update, 16 countries are now in Stage 2, and two countries―Kenya and Malawi―have entered Stage 3. Figure 2 shows the S-curve for each country using estimates ending with the year of their most recent survey. Projections are represented by the dotted lines.
Figure 2. Family Planning S-Curve Illustration for USAID Priority Countries in Sub-Saharan Africa, 1970 to 2020 and Projected Pathways Through 2030
Explore the data by selecting a country to see annual growth in mCPR. Select "Rapid Growth Stage 2 Countries" to highlight countries achieving average annual mCPR growth rates of 1.5 percentage points or higher. Select “See Countries with Projections Through 2030” to explore potential mCPR growth trajectories over the next decade under three scenarios, taking into account historic trends. The middle line represents the most likely trend to be achieved, in the absence of drastic changes. The highest and lowest lines represent the range that can be achieved with greater or reduced efforts.
Note: Data after 2020 are projected pathways using available survey data.
Sources: Data through 2019 are based on available survey data. Data for 2020-2030 are from the Track20 Family Planning Estimation Tool.
A wide range of growth patterns is evident among the countries in Stage 2. Countries such as Ethiopia and Zambia achieved rapid increases in mCPR over the last decade but may be seeing a slowing rate of increase as they approach Stage 3. Such countries may need to evaluate program priorities to match their context, including addressing obstacles to contraceptive continuation among current users, applying greater customization in service delivery approaches, and increasing investment in bringing services to hard-to-reach communities where demand for family planning has not yet been met.
Countries at the lower end of Stage 2, such as Mali and Niger, have not yet tapped into the potential for rapid mCPR growth but have an important window of opportunity to do so. Accelerated progress in such countries often begins with advocacy initiatives to generate high-level political support. All countries achieving rapid increases in mCPR during Stage 2 have made substantial investments in community-based distribution of family planning. Reaching Stage 2 of the S-curve does not guarantee rapid growth. The pace of growth depends on data-driven policy and program approaches that strategically and efficiently respond to increasing demand for family planning. Fluctuations in mCPR growth along each country’s curve underscores the importance of continuous program monitoring to identify periods of rapid, slow, or stagnating growth, and adapt interventions accordingly.
To better understand the different growth trajectories that countries may achieve during Stage 2, we can examine the examples of Ethiopia and Tanzania (see Figure 3 and Figure 4).
Figure 3. Ethiopia’s Family Planning S-Curve
Ethiopia provides an example of a country that successfully maintained rapid mCPR growth during Stage 2. As Ethiopia emerged from Stage 1, increases in mCPR followed a steep curve upward. This steep curve is a sign of a program that has efficiently and effectively met growing demand for family planning. Ethiopia’s significant investments in community-based distribution of family planning were likely a significant contributor to sustained rapid growth throughout Stage 2. As Ethiopia approaches Stage 3, greater investment in quality of care and supportive supervision of providers may help enhance client satisfaction with family planning services
Figure 4. Tanzania’s Family Planning S-Curve
Tanzania is an example of a slower increase in mCPR over time. Tanzania entered Stage 2 around 1998, nearly a decade ahead of Ethiopia. After a brief period of rapid increase, it maintained a more linear mCPR trend, with a flatter curve compared to Ethiopia’s exponential growth. Despite similar mean fertility ideals, demand for family planning satisfied by modern contraceptive methods is lower in Tanzania (53%) compared with Ethiopia (61%).
Each stage of the S-curve has different implications for family planning program priorities and goal setting. In Stage 1, countries may see the greatest returns on investment for interventions that address social norms around family planning use. With significant changes in mCPR are unlikely in this period, indicators measuring changes in demand for and access to family planning are important In Stage 2, decisionmakers may find it important to measure mCPR growth as a key program indicator as they monitor their performance in rapidly meeting growing demand, and they should complement this indicator with more person-centered program metrics discussed throughout this report. In Stage 3, goals and measurement strategies may shift to prioritize equity indicators and government financial commitments as countries at this stage work to attain long-term sustainability and equity across different subgroups.
Accelerating family planning programs' gains and strengthening their responsiveness to community priorities require greater availability and use of data for decision-making at subnational levels.
Future analyses of program performance will be more useful if examined at the lowest administrative unit for which reliable data are available. However, few nationally representative surveys have large enough samples for reliable estimates at the lowest administrative unit (often the district, county, or municipal level). To address these limitations for survey data, countries and donors can mobilize resources to increase surveys' sample size, but this approach is both time and cost intensive. Alternately, analysts can apply modeling approaches to existing survey data to generate estimates for small geographic units. Investing in this type of skills-building for data officers in ministries of health and national population councils will increase the usefulness of DHS data for subnational decision-making.
The limitations of data from nationally representative surveys also underscores the urgency of investment in robust health management information systems (HMIS). HMIS data are generated by health facilities at the local level, but concerns about data quality and consistency tend to limit their use in decision-making. Greater investment in and use of these data will lead to quality improvements. High-quality HMIS data are essential to locally driven and highly customized programs that will be more responsive to clients’ needs and priorities.
Most countries in sub-Saharan Africa saw little increase in contraceptive use among adolescents, but opportunities for expanded use in this age group vary by country.
Ensuring that young people have access to high-quality sexual and reproductive health information and services, including contraceptives, supports them in achieving their personal, professional, and reproductive goals. The global family planning community broadly recognizes that youth have unique needs and challenges when it comes to contraception compared with older women. As such, countries around the world have committed to promoting youth’s rights to sexual and reproductive health services. However, community opposition to sexual activity among unmarried youth and expectations to prove fertility soon after marriage remain constraints in many contexts.
While global initiatives increasingly prioritize youth, opportunities for increasing mCPR among this group may be limited. To provide additional context, we examined mCPR by age (looking at both adolescents ages 15 to 19 and youth ages 15 to 24), marital status, and sexual activity (see Figure 5). These additional dimensions can help decisionmakers understand the potential for continued contraceptive uptake among this demographic. Marital status and sexual activity among young women ages 15 to 24 and adolescents ages 15 to 19 vary significantly by country, potentially reflecting country-specific patterns around age of marriage and nonmarital sex. These factors influence contraceptive uptake, particularly for adolescent girls ages 15 to 19.
Figure 5. mCPR Disaggregated by Age Group (15-19 and 20-24), Marital Status, and Recent Sexual Activity in Selected Countries Shows Variation in Country Patterns
Source: Demographic and Health Surveys. Data are drawn from the two most recent surveys.
On average, the lowest mCPR is among adolescent girls ages 15 to 19. In countries like Ethiopia, Rwanda, and Senegal, where more than 75% of girls ages 15 to 19 report that they have never had sex, it is to be expected that mCPR rates are low. In comparison, countries where more than half of adolescent girls report having ever had sex―such as Côte d'Ivoire, Liberia, Malawi, and Mozambique―may have a higher need for expanded family planning programming to address adolescent health needs, especially since these countries generally experience high rates of adolescent pregnancy.
In nine countries (Côte d’Ivoire, Guinea, Liberia, Madagascar, Malawi, Mali, Mozambique, Niger, and Zambia), more than 25% of all adolescent girls ages 15 to 19 have begun childbearing. In the majority of countries (15), more than 25% of sexually active unmarried adolescent girls have begun childbearing; and in six of those countries (Côte d’Ivoire, DRC, Ghana, Liberia, Mozambique, and Togo) the proportion of adolescent girls who report being “sexually active, unmarried” is over 10%. While more than 65% of sexually active unmarried adolescent girls have begun childbearing in Niger and Senegal, the proportion of adolescent girls who report being “sexually active, unmarried” is less than 1% in both countries (see Figure 2). These countries may choose to prioritize major initiatives addressing comprehensive sexuality education, body awareness, and contraceptive access and uptake among youth, particularly among adolescents.
Table 2. Percent of Adolescent Girls Ages 15-19 Who Have Begun Childbearing, by Marital Status and Sexual Activity
| Country | Adolescent girls ages 15-19 | Sexually active unmarried | Married/ in union |
|---|---|---|---|
| Benin | Proportion of the population | 11% | 19% |
| Begun childbearing | 14% | 84% | |
| Burkina Faso | Proportion of the population | 5% | 32% |
| Begun childbearing | 15% | 67% | |
| Cote d'Ivoire | Proportion of the population | 19% | 21% |
| Begun childbearing | 26% | 86% | |
| DRC | Proportion of the population | 12% | 21% |
| Begun childbearing | 27% | 77% | |
| Ethiopia | Proportion of the population | 2% | 17% |
| Begun childbearing | 52% | ||
| Ghana | Proportion of the population | 11% | 6% |
| Begun childbearing | 26% | 81% | |
| Guinea | Proportion of the population | 6% | 28% |
| Begun childbearing | 21% | 76% | |
| Kenya | Proportion of the population | 1% | 12% |
| Begun childbearing | 32% | 84% | |
| Liberia | Proportion of the population | 24% | 12% |
| Begun childbearing | 33% | 79% | |
| Madagascar | Proportion of the population | 7% | 34% |
| Begun childbearing | 38% | 69% | |
| Malawi | Proportion of the population | 6% | 24% |
| Begun childbearing | 33% | 83% | |
| Mali | Proportion of the population | 6% | 42% |
| Begun childbearing | 29% | 74% | |
| Mozambique | Proportion of the population | 13% | 37% |
| Begun childbearing | 30% | 73% | |
| Niger | Proportion of the population | 0.1% | 61% |
| Begun childbearing | 66% | 64% | |
| Nigeria | Proportion of the population | 4% | 23% |
| Begun childbearing | 13% | 74% | |
| Rwanda | Proportion of the population | 1% | 2% |
| Begun childbearing | 34% | 87% | |
| Senegal | Proportion of the population | 0.2% | 21% |
| Begun childbearing | 66% | 58% | |
| Tanzania | Proportion of the population | 7% | 23% |
| Begun childbearing | 29% | 80% | |
| Togo | Proportion of the population | 11% | 13% |
| Begun childbearing | 14% | 86% | |
| Uganda | Proportion of the population | 5% | 20% |
| Begun childbearing | 32% | 83% | |
| Zambia | Proportion of the population | 8% | 15% |
| Begun childbearing | 48% | 89% |
Source: Demographic and Health Surveys
* DHS Statcompiler, most recent DHS. All variables were not available for 2019 Ethiopia mini-DHS, so the 2016 Standard DHS was used.
** Most recent DHS. All variables were not available for 2019 Ethiopia mini-DHS, so the 2016 Standard DHS was used.
Strong performance in key family planning program dimensions, especially related to data collection and use, is associated with increases in mCPR.
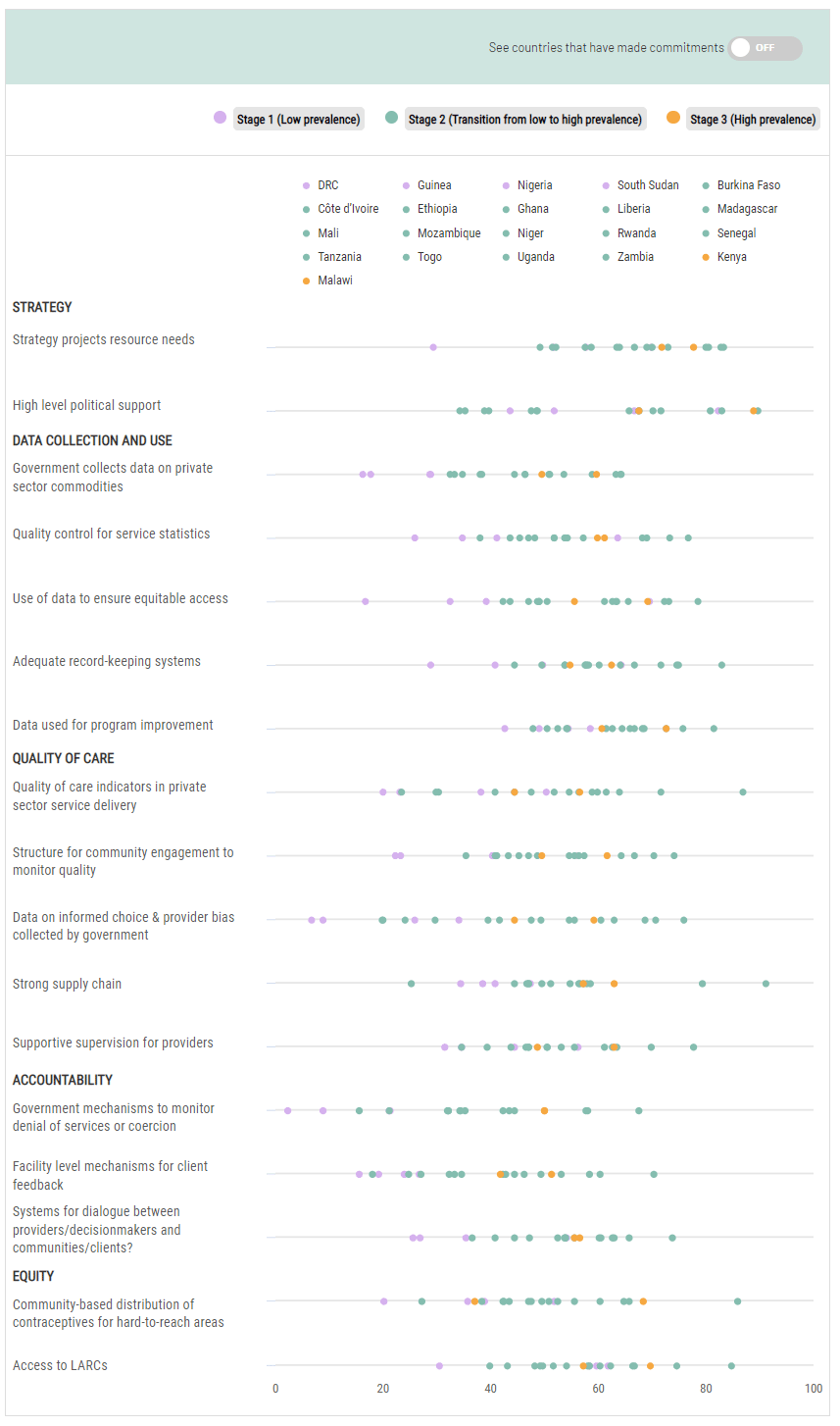
To better understand the factors that may support or hinder increased access to and use of family planning across countries, we analyzed 17 measures included in the National Composite Index for Family Planning (NCIFP) for 21 of the 22 priority countries (NCIFP scores for Benin were excluded due to data quality concerns). The NCIFP is a tool developed to support decisionmakers as they work to improve the enabling environment for family planning, focusing on five dimensions of national programs―Strategy, Data Collection and Use, Quality of Care, Accountability, and Equity―each comprising a set of items against which country stakeholders score themselves.c
NCIFP scores are gathered from national family planning experts across government, the private sector, nongovernmental and faith-based organizations, academic and research organizations, donor-assisted projects, and other influential actors. An analysis of global NCIFP scores globally demonstrates that higher scores are associated with higher mCPR, and that this relationship between programmatic performance and mCPR is more robust in SSA countries (see Figure 6).
Figure 6. NCIFP Ratings and mCPR Are Associated Globally, Especially in Sub-Saharan Africa
Source: PRB analysis of National Composite Index for Family Planning (NCIFP) 2017.
We examined FP2020 commitments as well as NCIFP scores in 2017. We further examined changes in scores between 2014 and 2017 for the indicators with data available for both years.
Across SSA, countries largely achieved improvements in dimensions for which FP2020 commitments were made. However, commitments were not exclusively associated with areas of program progress. Many countries achieved high scores in the Strategy dimension, which may have been supported by the push to develop costed implementation plans through the FP2020 partnership. Yet, several countries (Burkina Faso, Côte d'Ivoire, Madagascar, Mali, Niger, Senegal and Togo) have low scores in the Strategy item on high-level leadership and support for the family planning program.
While just half of countries made FP2020 commitments around Data Collection and Use, most countries had high scores in this dimension. But data challenges persist. In particular, countries score poorly on government collection of data from private sector providers, including on supply availability. Liberia is an exception; the government collects and integrates data on private sector commodities within the national logistics management information system (LMIS) to inform supply forecasting.
Quality of Care commitments and scores vary across countries. However, all countries except Burkina Faso and Tanzania reported lower scores in quality of care in the private sector compared with the public sector. This finding warrants further investigation to assess the extent to which it holds true across and within countries (for example, do quality of care scores in the private sector differ in urban versus rural settings and by the type of private sector provider). While nearly all countries pledged to increase private sector involvement or partnership, few countries identified specific actions or data needed to ensure high-quality services in private facilities. Malawi’s report to FP2020 notes that while the need to assess quality of care in the private sector is well established, private hospitals and pharmacies have no process available to them to report service statistics to the government.
Some countries did identify actionable steps to address quality of care in the private sector. After the Ghana Health Service committed to include DMPA-SC (a self-injected contraceptive method) in the method mix available at health facilities, the government supported master trainers in both the public and private sectors to coach providers on how to dispense the method. Guinea, Liberia, and Kenya committed to investments in capacity strengthening for providers in both the public and private sectors. Senegal pledged to revise laws governing family planning service provision by pharmacists. Notably, Malawi made a commitment to develop national supervision standards that include service providers’ accountability and quality of care measures.
While all countries committed to improving their logistics system and strengthening provider training, scores for both varied significantly, with nearly half of countries scoring below-average in each metric. Scale-up of digital technologies that strengthen LMIS, such as OpenLMIS, can generate time, cost, and management efficiencies that streamline procurement and reduce contraceptive stockouts.
Most countries had low or declining scores for collection of data on informed choice and provider bias, as well as the existence of systems for dialogue between clients and health providers or local officials on family planning services. For instance, DRC reported that, while it has no formal feedback system, client comments are collected through suggestion boxes available at some facilities. Ghana also uses suggestion boxes at facilities and implements periodic client exit interviews and surveys by health facility staff and district and regional health management teams. Togo conducts an annual survey on the availability of family planning products and services, as well as client satisfaction with services. The survey results are analyzed and disseminated to all regions to inform development and implementation of annual workplans. Relatedly, scores for the Accountability dimension are lowest across the board. Of particular note, few countries report that structures exist for clients to report denial of services or for regular program review of violations of rights or choice. Establishing or strengthening formal mechanisms to protect choice and promote dialogue will require dedicated attention and investment and must be prioritized in national and subnational strategies. Country stakeholders report challenges funding accountability structures when service delivery interventions are already underfunded. In such resource-constrainted environments, digital technologies that generate time and cost efficiencies may help create space in budgets for investment in essential accountability structures. In addition, digital approaches like PartME model, operating at scale in Ghana, can be used for cost-efficient accountability platforms that support community dialogue with decisionmakers.
Within the Equity dimension, scores for community-based distribution (CBD) mechanisms are especially revealing. While nearly all countries made FP2020 commitments related to establishing or scaling-up community-based distribution programs, scores for this item were often low or stagnant, with high scores over 65 points only seen in Ethiopia, Malawi, and Rwanda. These three countries also received relatively high scores for their logistics systems, while the opposite was true for South Sudan, Côte d'Ivoire, and DRC. Other factors that affect effective CBD programs include the lack of staff (in part due to high turnover), the need for trained personnel, and limited resources to cover wide and often remote geographic areas.
To better understand the programmatic factors associated with increases in mCPR, we further categorize countries by S-curve stage (see Figure 7).
Figure 7. NCIFP Scores for Selected Countries in Sub-Saharan Africa by S-Curve Stage, 2017
Hover over a country to see its performance across selected NCIFP items, either for all countries or for those that made an FP2020 commitment related to that item.
Fully interactive version available on dekstop
| See countries that have made commitments | ||||||||||
|
STRATEGY
Strategy projects resource needs High level political support DATA COLLECTION AND USEGovernment collects data on private sector commodities Quality control for service statistics Use of data to ensure equitable access Adequate record-keeping systems Data used for program improvement QUALITY OF CAREQuality of care indicators in private sector service delivery Structure for community engagement to monitor quality Data on informed choice & provider bias collected by government Strong supply chain Supportive supervision for providers ACCOUNTABILITYGovernment mechanisms to monitor denial of services or coercion Facility level mechanisms for client feedback Systems for dialogue between providers/decisionmakers and communities/clients? EQUITYCommunity-based distribution of contraceptives for hard-to-reach areas Access to LARCs |
||||||||||
Source: National Composite Index for Family Planning (NCIFP) 2017.
Countries in Stage 1 had low ratings for most NCIFP items outside of the Strategy dimension.
Scores around Data Collection and Use were positively associated with increases in mCPR.
Stage 1 countries largely scored over 50, Stage 2 countries scored between 50 to 60 (except Rwanda, a strong performer with scores over 80), and Stage 3 countries scored over 60. Stage 3 countries (Kenya and Malawi) and Rwanda were the only countries to score above average in the Accountability dimension. The other 17 countries scored below average in the item structures to report denial of services on non-medical grounds (such as age or marital status). While many countries have policies against denial of service on such grounds, they may lack the infrastructure to support accountability.
The rights-based orientation of family planning programs in all of the SSA countries we reviewed, even countries with comparatively high scores in Accountability, must be strengthened through policy and program mechanisms that protect choice and equity. Official policy avenues for documenting, reporting, and using information on rights and choice in family planning programs should be accompanied by public communication initiatives that inform communities and individuals―as well as frontline providers―that client choice is a fundamental cornerstone of the family planning program and that advertise and encourage confidential reporting of issues or violations, including refusal to remove methods or denial of services based on age or spousal consent. Digital reporting tools highlighted in this report may serve as effective and confidential platforms for clients to report service issues ranging from limitations in choice (for example, reporting lack of availability of preferred methods) to experiences of discrimination or denial of services and violations of rights. Providers may also be encouraged to report on structural limitations to the provision of client-centered, rights-based services (for example, documenting when they are unable to provide a preferred method to a client due to lack of supplies or training).
Family planning programs may be better assessed through person-centered metrics, despite the limitations of available metrics.
Weak performance in the NCIFP Accountability dimension may reflect, at least in part, family planning programs’ emphasis on population-level contraceptive uptake rather than person-centered, rights-based service provision. Calls to reimagine this approach to benchmarking the success of family planning programs are leading to the collection and analysis of new and/or refined metrics that emphasize client autonomy and quality of care. This reimagining includes overdue efforts to better define and measure women’s “need” or “demand” for family planning, recognizing that intention to avoid pregnancy is not synonymous with wanting to use contraception.5
Even as efforts to systematically integrate more person-centered metrics in nationally representative data collection continue, decisionmakers can immediately act to ensure metrics beyond mCPR are used to assess the robustness of family planning programs. Table 3 presents DHS metrics addressing demand for family planning satisfied with any contraceptive method, the proportion of women who were counseled about potential side effects when accessing their current method, and the proportion of women—among those who do not want more children—who do not intend to use contraception.
These metrics retain significant limitations. The metric of demand satisfied arguably conflates wanting to avoid pregnancy with wanting to use contraception. Counseling about side effects is just one feature of high-quality, client-centered counseling. A lack of intention to use family planning among women who do not want to become pregnant may be a signal of women executing their right not to use contraception regardless of their pregnancy intentions, or it may be a signal of reproductive coercion by partners, parents-in-law, or others. Still, these metrics, among others, may contribute to reframing how program progress is conceptualized to better serve the reproductive, personal, and professional needs and preferences of family planning clients.
Table 3. Demand for Family Planning Satisfied, Counseling on Side Effects, and Intention Not to Use Family Planning, by S-Curve Stage
| S-curve stage | DHS | Country | Demand satisfied (all methods, all women)* | Told about side effects (all users)* | Does not intend to use contraception in the future, among women who do not want more children (all women)** |
|---|---|---|---|---|---|
|
Stage 1 - Low Prevalence
|
2018 | Benin | 36% | 62% | 54% |
| 2018 | Guinea | 40% | 59% | 71% | |
| 2017-18 | Nigeria | 49% | 74% | 55% | |
| Stage 2 - Transition from Low to High Prevalence | 2013-14 | Burkina Faso | 43% | 74% | 45% |
| 2018 | Cote d'Ivoire | 46% | 45% | 50% | |
| 2012 | DRC | 46% | 60% | 47% | |
| 2011-12 | Ethiopia | 63% | 46% | 42% | |
| 2013-14 | Ghana | 52% | 67% | 50% | |
| 2019-20 | Liberia | 50% | 69% | 44% | |
| 2019 | Madagascar | 67% | 61% | 38% | |
| 2010 | Mali | 43% | 68% | 53% | |
| 2014 | Mozambique | 37% | 62% | 48% | |
| 2011 | Niger | 47% | 44% | 60% | |
| 2015 | Rwanda | 81% | 61% | 22% | |
| 2016 | Senegal | 56% | 86% | 40% | |
| 2008-09 | Tanzania | 66% | 62% | 32% | |
| 2016 | Togo | 43% | 80% | 46% | |
| 2018 | Uganda | 60% | 67% | 32% | |
| 2019-20 | Zambia | 69% | 82% | 32% | |
|
Stage 3 - High Prevalence
|
2014 | Kenya | 77% | 60% | 24% |
| 2015-16 | Malawi | 75% | 78% | 21% |
Source: Demographic and Health Surveys.
The COVID-19 pandemic reinforces the importance of investment in country data systems that are resilient to shocks.
The COVID-19 pandemic is the most significant potential disruptor to family planning programs since the last review. At the pandemic’s onset in March 2020, many experts predicted stalls in family planning program progress, including substantial declines in contraceptive use and increases in unmet need and unintended pregnancy.6
Analyzing pandemic-related disruptions in family planning programs proved challenging, as countries struggled with conducting data collection (including for the DHS). Data collected through national HMIS became a key early source of information on potential disruptions. In March 2021, findings from a convening examining HMIS data from multiple countries indicated that, for the most part, family planning services experienced a brief period of acute disruption but quickly recovered. The timing, speed, and scale of this recovery varied, with disruptions persisting or recurring across some countries, like Niger, over multiple cycles.
Emerging data on pandemic-related disruptions are largely reinforcing these early findings. For example, an analysis of survey data from six SSA countries (Burkina Faso, Côte d'Ivoire, DRC, Kenya, Nigeria, and Uganda) implemented between June 2020 and February 2021 confirm that disruptions were largely temporary and well below initial estimates. However, the ongoing pandemic could lead to future disruptions, whether driven directly by the pandemic or indirectly by resulting shortfalls in domestic financing for family planning. On the other hand, the pandemic also created a window for innovation, including accelerated adoption of digital technologies in family planning programs, which may have contributed to family planning program resilience. Successful programmatic adaptations―including virtual training for providers, online marketplaces supporting client self-care, and telehealth approaches to family planning service delivery―may enhance program impact and efficiency beyond the pandemic.
While disruptions in service delivery were more limited than originally feared, disruptions in data collection have been extensive and remain ongoing as the pandemic enters its third year. The pandemic halted new DHS across the globe because of health and safety concerns. Other surveys were stalled or conducted with limited and potentially biased samples (such as surveys implemented by phone, which may disproportionately reach women with higher incomes).
These disruptions have drawn attention to the importance of having strong country data collection systems, particularly HMIS, that are resilient to health system shocks.
While the limitations of HMIS data are well recognized―including challenges around data quality, accuracy, and fragmentation―findings from analyses of HMIS data during the pandemic are increasingly being verified by survey findings. Countries are leading efforts to address HMIS challenges, and these efforts should be met by commitment and investment from the donor community.
Family planning financing is vulnerable heading into the next decade.
At the time of the last report, donor funding for family planning had increased steadily between 2008 and 2014. While USAID remained the largest bilateral donor for family planning assistance in low- and middle-income countries, the governments of the United Kingdom and France became larger actors in the space.
In the intervening years, domestic resource expenditure for family planning appears to be increasing, although refinements in how such expenditures are tracked limit the extent to which changes over time can be clearly assessed. In the same period, donor commitments (including bilateral, multilateral, and private commitments) to family planning assistance in SSA have stagnated (see Figure 8).
Figure 8. Official Donor Commitments to Family Planning and Reproductive Health in Sub-Saharan Africa, 2010-2019 ($USD millions)
Source: Organisation for Economic Co-operation and Development, QWIDS (Query Wizard for International Development Statistics), data accessed as of March 17, 2022.
A 2020 Kaiser Family Foundation analysis of bilateral donor funding among 10 major donors shows continued declines as of that year. Decreases in bilateral assistance are largely driven by the United Kingdom because of pandemic-related constriction in their overall economy.
Investments in domestic resource mobilization, led by policymakers and civil society across countries in SSA, have generated new or increased financial commitments for family planning. However, sustaining both donor and country financial commitments over the next decade may be challenging as the pandemic’s economic effects continue to influence national economies. In this context, it is essential for family planning programs to identify and integrate approaches that increase efficiencies in implementation, including scale-up of proven digital solutions.
